Researchers share findings on COVID-19's impact on occupational disruption and chronic disease
Author: UNB Research
Posted on Apr 9, 2021
Category: Publications , COVID-19 , Research

Around the world, researchers across different fields and disciplines are working to address the challenges, issues and implications of the 2019 novel coronavirus pandemic. Here at UNB, our own research community is part of that global movement.
Last year, we introduced you to 13 new, funded COVID-19 research projects and their teams; now, with a full year of pandemic life behind us, we’re checking in to see what they’re working on and what they’ve accomplished. Want catch up with the other teams? Keep an eye on this page for updates!
In this story, we visit the Centre for Research in Integrated Care (CRIC) on UNB’s Saint John campus, where researchers Dr. Kerrie Luck and Dr. Shelley Doucet examined the experience of occupational disruption among individuals living with chronic disease during the COVID-19 pandemic.
Specifically, they focused on people’s experiences managing disease(s) and accessing routine healthcare during a health crisis.
What is Occupational Disruption? Dr. Luck provided a definition for this concept:
Occupation is commonly defined as everyday activities to occupy time and bring purpose to life. These activities can include self-care (e.g., healthy eating, exercising), leisure (e.g., socializing with friends and family), and/or productivity (e.g., work outside home, volunteering). Occupation is believed to give life meaning and organize behavior, and is also a critical determinant of health and wellbeing with therapeutic potential. While some occupations may be easily adjusted or omitted, individuals can experience occupational disruption if they cannot participate in the day-to-day activities that make up life as they know it, as is the case in a pandemic.
The research Dr. Luck and Dr. Doucet conducted offers a first glimpse into this concept as it relates to a pandemic and has identified how reactions to occupational disruption have influenced behavior and contributed to an apprehension in seeking health services. The project also highlighted the need for better communication, awareness and research around existing precautionary strategies to protect people using the healthcare system and the system’s capacity to treat non COVID-19 related medical issues.
“Exploring these obstacles and involving those with lived experience in policy development and implementation, will ensure their voices are heard, help mitigate risk and ultimately improve occupational performance,” said Dr. Luck.
Their qualitative, descriptive study invited 23 New Brunswickers living with chronic disease to participate in in-depth, semi-structured interviews.
The study identified three main themes and seven sub-themes:
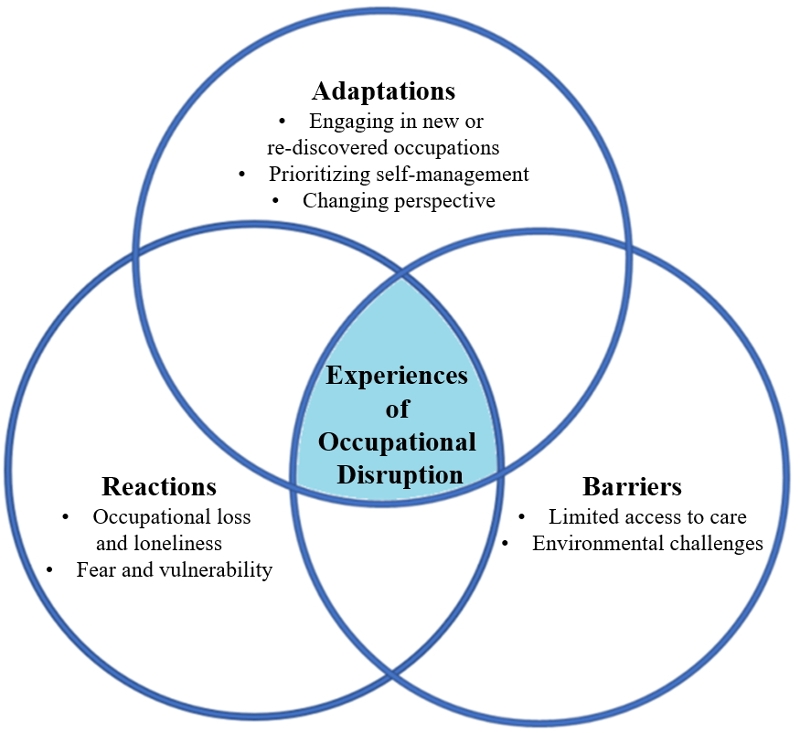 Reactions
Reactions
- occupational loss and loneliness
- fear and vulnerability
Adaptations
- engaging in new or re-discovered occupations
- prioritizing self-management
- changing perspective.
Barriers
- limited access to care
- environmental challenges
Their findings show how individuals living with chronic disease adapted their activities to provide structure and purpose in response to restrictions imposed by the pandemic. Notably, participants reported “heightened engagement in occupations focusing on maintaining health and wellbeing,” according to Dr. Luck.
“To fully enable these positive impacts,” adds Dr. Luck “not only is it important for individuals to adapt to achieve these occupations, but it is imperative that social support and resources are put in place to assist with behavior change.”
However, not all adaptations were positive.
These new changes in the environment also created obstacles for participants as feelings of fear and vulnerability contributed to an apprehension in seeking medical care. Most participants did not want to go into a healthcare building feeling they would be in contact with other “sick” people and it would put them at higher risk for being exposed to COVID-19. As one participant explained, “I don't wanna go to a hospital…if you're sick [COVID-19], that's where you’re going to go”.
Due to these fears, many put off seeking care when they would normally acquire it. Some also reported they didn’t know if they would have even been seen, due to the system being overburdened with COVID-19.
“If this maladaptive strategy of avoidance to seek healthcare is not addressed, it could cause significant harm,” says Dr. Luck.
The researchers also highlighted the need for future research in patient self-management in the current COVID-19 environment, and the need for policy to support these practices.
“This would help individuals living with chronic disease enhance their adaptive strategies and regain control, build routines and manage wellness,” says Dr. Luck. “It can also be an opportunity for healthcare professionals to intervene and support those interested in positively changing behaviors.”
Dr. Luck and Dr. Doucet are currently working on sharing their insights and findings with stakeholders.
They have published an article on their project in the Journal of Occupational Science, and have also developed a slate of knowledge translation media to help share their findings more broadly.
Click here to see the poster summarizing their findings.
Click here to watch a short video about their findings.
This research is funded by the New Brunswick Innovation Foundation, the New Brunswick Health Research Foundation, and the Atlantic Canada Opportunities Agency as part of a special COVID-19 funding program.
Media: If you are interested in this story, and would like more information, please contact Jeremy Elder-Jubelin, Marketing and Communications Officer in the Office of Research Services.
More information:
Dr. Shelley Doucet | Centre for Research in Integrative Care | Nursing and Health Sciences (Saint John)
Research at UNB | Graduate Studies at UNB | Postdoctoral fellowships
About the researchers:
Dr. Kerrie Luck recently completed a postdoctoral fellowship with the Centre for Research in Integrated Care (CRIC) at UNB in Saint John. She is an occupational therapist with research interests that include tobacco reduction and policy; program design and evaluation; and healthcare and service delivery.
Dr. Shelley Doucet is the Jarislowsky Chair in Interprofessional Patient-Centred Care, an associate professor in Nursing, and director of the Centre for Research in Integrated Care at the University of New Brunswick. She is also the co-founder and co-director of NaviCare/SoinsNavi, the New Brunswick navigation centre for children and youth with health care needs, an example of one of these integrated care solutions.
Related Pages: Where are they now? COVID-19 researchers update us on their progress